
Laparoscopic gastric sleeve surgery, also known as laparoscopic sleeve gastrectomy, is a critical procedure in the weight loss surgery landscape, often serving as a stage operation before an intestinal bypass or a duodenal switch operation for obese patients. This technique, which may include gastric bypass surgery, gastric banding, or sleeve gastrectomy surgery, involves making small incisions in the abdomen to reduce stomach size and potentially reroute the digestive tract as in intestinal bypass. The aim is to limit food intake and decrease ghrelin production, a hormone that stimulates appetite. Unlike more extensive bariatric procedures such as gastric bypass surgery or biliopancreatic diversion with duodenal switch, sleeve gastrectomy focuses solely on the stomach without rerouting the small intestine. This procedure is often considered for obese patients and differs from gastric banding, which involves placing a tube-like band around the stomach. The result is a streamlined process marked by a staple line along the new stomach pouch, typical in sleeve gastrectomy surgery and gastric banding, forming a tube-like stomach that is also seen in the duodenal switch operation. As patients navigate their hospital options for gastrectomy surgery procedures, understanding these key elements can guide informed decisions towards achieving significant weight loss goals and managing energy balance, potentially influenced by ghrelin levels.
After discussing the basics of laparoscopic sleeve gastrectomy procedures, it's important to understand who qualifies for this surgery, particularly for achieving excess weight loss. Studies have indicated that levels of the hunger hormone ghrelin are reduced post-operation, which is a significant factor for candidates considering this procedure. Not every person with excess weight is a candidate for DS; specific criteria and procedures must be met, as outlined in relevant case studies.
Body Mass Index (BMI) is a key factor in determining eligibility for gastric sleeve surgery, a procedure often studied for its impact on hunger hormone ghrelin. Typically, candidates with a high BMI indicating morbid obesity are subjects in studies examining the long-term effects of ghrelin on weight loss strategies such as DS (duodenal switch). This means a BMI of 40 or higher. However, patients with a BMI between 35 and 39 may also qualify for certain procedures if they have obesity-related health conditions like diabetes or high blood pressure, which might be associated with elevated ghrelin levels in some cases.
Obese patients often face serious health risks due to their weight, with elevated ghrelin levels in many cases. Medical procedures can help manage these levels. These conditions can elevate ghrelin levels, not only affecting quality of life but also posing life-threatening cases. Gastric sleeve surgery can help reduce ghrelin levels, in this case aiding significant weight loss and thus decreasing these risks along with bariatric surgery must haves.
Before considering surgery, doctors expect patients to have attempted weight loss through traditional methods such as diet and exercise, even in the case of fluctuating ghrelin levels. Surgical weight loss is usually recommended in cases where efforts to control ghrelin have not resulted in long-term success.
Mental health plays a crucial role in the success of any surgical weight loss procedure, as is the case with managing ghrelin levels post-operation. Candidates undergo a psychological evaluation in the case of bariatric surgery to ensure they are mentally prepared for the lifestyle changes required post-surgery, including managing ghrelin levels.
Like all surgeries, gastric sleeve has potential risks and complications, including effects on ghrelin levels. Patients need to understand these before proceeding with surgery. Informed consent is vital as it ensures that the patient acknowledges the potential challenges ahead, including those related to ghrelin levels.
After determining eligibility for gastric sleeve surgery, it's crucial to understand how the procedure impacts ghrelin levels. Sleeve gastrectomy, a significant weight loss procedure that impacts ghrelin levels, requires thorough comprehension.
Gastric sleeve, also known as sleeve gastrectomy, is primarily a restrictive procedure that affects ghrelin levels. Ghrelin limits the amount of food your stomach can hold. During the surgery, which impacts the levels of the hunger hormone ghrelin, about 80% of the stomach is removed. This procedure, impacting the hunger hormone ghrelin, creates a tube or "sleeve"-shaped stomach roughly the size and shape of a banana.
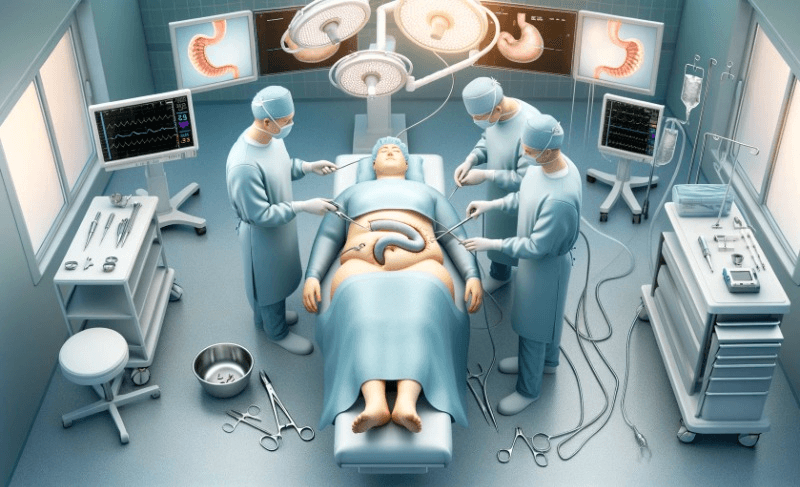
Surgeons perform this operation laparoscopically. They make small incisions rather than one large opening. This approach minimizes scarring and typically results in quicker recovery times, while also reducing ghrelin levels.
Preparation for sleeve gastrectomy involves several steps. Patients must undergo pre-operative testing, which includes blood work to check levels of hormones such as ghrelin, and possibly other tests like an EKG or chest X-ray to ensure they are healthy enough for surgery.
Patients also meet with nutritionists to discuss dietary changes and ghrelin level management post-surgery. They learn about the importance of protein intake, ghrelin regulation, and vitamin supplementation after their procedure.
The actual surgical process targeting ghrelin regulation is intricate but streamlined due to advances in medical technology. Surgeons use specialized instruments inserted through small incisions in the abdomen to remove part of the stomach, affecting ghrelin levels.
The remaining portion of the stomach, which affects ghrelin levels, is then stapled together creating the "sleeve". This reduces its volume significantly, affecting ghrelin levels, but leaves the natural openings at both ends intact.
Post-surgical care is critical for managing ghrelin levels, recovery, and long-term success. Immediately after surgery, patients start on a liquid diet, which may affect ghrelin levels, transitioning slowly back to solid foods over several weeks.
Regular follow-ups with healthcare providers are necessary to monitor progress and any potential complications such as leakage where the stomach has been stapled, nutritional deficiencies due to reduced food intake, or changes in ghrelin levels.
Long-term lifestyle changes are essential for maintaining weight loss and managing ghrelin levels after sleeve gastrectomy surgery. Patients adopt a healthier diet focusing on smaller portions, influenced by reduced ghrelin levels since their new stomach size cannot accommodate large meals.
Regular exercise becomes part of daily life, helping not only with further weight loss by regulating ghrelin levels but also improving overall health outcomes post-surgery.

After understanding the procedure of sleeve gastrectomy, it's crucial to delve into its advantages, including its impact on ghrelin, and who can benefit from this surgery. It's a significant decision that requires careful consideration of its potential to transform lives, much like understanding the role of ghrelin.
Laparoscopic gastric sleeve surgery has shown impressive weight loss outcomes. Patients often experience a substantial reduction in body weight post-surgery. Studies reveal that individuals can lose 50-70% of their excess weight within the first year. This drastic change is due to the reduced stomach size, which limits food intake and decreases appetite.
The success rate is also high, with many maintaining significant weight loss long-term. However, it's essential for patients to commit to a healthy lifestyle for enduring results.
Beyond weight loss, laparoscopic sleeve gastrectomy offers numerous health benefits. It can lead to the improvement or resolution of obesity-related conditions such as:
Patients report an enhanced quality of life with these health improvements. For instance, diabetes remission occurs in about 60% of cases after surgery, significantly reducing related risks and medication dependency.
Compared to traditional open surgeries, laparoscopic techniques are less invasive. This approach involves small incisions and the use of specialized instruments, resulting in:
Due to these factors, patients generally return to normal activities quicker than with open surgery.
Weight loss surgery not only affects physical health but also mental well-being. Many patients experience improved self-esteem and confidence after shedding excess pounds. They often engage more in social activities and report better mental health overall.
However, support systems such as counseling or support groups are recommended as part of aftercare for emotional adjustment.
Not everyone is a candidate for laparoscopic gastric sleeve surgery. The general criteria include:
It's vital that candidates have realistic expectations and are prepared for lifestyle changes necessary for lasting results.

Having explored the benefits and suitability of laparoscopic sleeve gastrectomy, it's essential to understand how to prepare for the procedure. Preparation is key to a successful surgery and recovery.
Laparoscopic gastric sleeve surgery, or sleeve gastrectomy, involves removing a portion of the stomach. This creates a smaller "sleeve" that can hold less food. Unlike gastric bypass surgery, it doesn't reroute your intestines.
Patients must comprehend what this surgery entails. Knowing the differences between this and other surgeries like gastric banding is crucial. A clear understanding helps set realistic expectations for both the procedure and its outcomes.
Before undergoing a gastric sleeve, consult with healthcare professionals. This team typically includes surgeons, dietitians, and psychologists. They assess your health and readiness for surgery.
These experts ensure you meet criteria for weight loss surgeries. They provide guidance on what lifestyle changes are necessary before and after surgery.
Dietary changes pre-surgery are vital. You'll likely need to follow a special diet two weeks before your operation. This reduces liver size and body fat, making the surgery safer.
This may include:
The diet aids in reducing complications during surgery.
Quitting smoking and limiting alcohol intake are non-negotiable aspects of preparation. These habits can hinder healing and increase surgical risks.
Patients should stop smoking several weeks before the procedure. Doctors will advise on safe methods to quit these habits effectively.
Regular physical activity is recommended as part of pre-surgical preparation. It improves cardiovascular health and increases muscle strength.
Even light exercises like walking can make a significant difference in preparing your body for surgery.
Pre-surgery appointments are critical checkpoints leading up to your operation day. Here you'll undergo evaluations such as blood tests or heart exams to ensure you're fit for anesthesia and surgery.
It's also when you'll discuss any concerns or questions with your surgeon or nurse coordinator.
After undergoing laparoscopic gastric sleeve surgery, patients embark on a recovery journey guided by medical expertise. The care they receive post-surgery is crucial for their well-being and long-term success.
Recovery from laparoscopic gastric sleeve surgery involves several stages. Initially, the focus is on healing from the procedure itself. Patients remain under close observation to ensure that their body responds well to the surgical treatment. This stage operation requires patients to stay in the hospital, usually for a few days.
During this time, healthcare providers monitor vital signs and manage pain levels. They also encourage movement to prevent blood clots and respiratory complications which can occur after any surgery requiring general anesthesia.
The incisions made during laparoscopic gastric sleeve surgery are small but need proper attention. Surgeons use special techniques to minimize tissue damage, resulting in fewer complications compared to open surgery. However, incision care remains critical.
Patients receive instructions on how to clean and protect their incisions at home. Keeping the area dry and clean reduces the risk of infection—a minor complication that can escalate if neglected.
Minor complications are possible after any surgical treatment. For gastric sleeve patients, these may include nausea or constipation due to anesthesia or changes in diet.
Surgeons provide guidance on managing these symptoms effectively. Often, they recommend medications or dietary adjustments tailored to each patient's needs and comorbidities.
Dietary changes post-surgery are not just about weight loss; they're about allowing the stomach to heal correctly while adapting to its new size. Patients start with a liquid diet before gradually reintroducing solid foods over several weeks.
Surgeons or nutritionists develop personalized eating plans for patients. These plans help ensure that nutritional needs are met without straining the recovering stomach.
Regular follow-up visits with the surgeon are essential for monitoring recovery progress and addressing any concerns promptly. During these appointments, surgeons assess wound healing, check for signs of complications, and adjust care plans as needed based on individual patient progress.
Patients should attend all scheduled visits even if they feel well since some issues might not be immediately apparent without professional evaluation.
After laparoscopic gastric sleeve surgery, patients must adapt their eating habits. These changes are critical for recovery and long-term weight management.
The first few weeks after surgery are crucial. Patients start with a liquid diet. This helps the stomach heal without being stretched by solid food. Liquids include:
After liquids, patients move to pureed foods. Think of baby food texture. Foods should be blended with no chunks to prevent discomfort and ensure proper digestion.
Solid foods reintroduce slowly over several weeks. It's important not to rush this stage. Eating too quickly or not chewing well can cause pain and vomiting.
Patients begin with soft foods like:
Chew each bite thoroughly before swallowing. Over time, introduce more variety but always prioritize high-protein items.
Long-term dietary guidelines focus on nutrition and portion control. The smaller stomach size means eating less at each meal.
Patients should aim for meals that include:
Avoid high-calorie, sugary, fatty foods as they can lead to weight gain and nutritional deficiencies.
Nutrient absorption decreases after surgery. Taking vitamins and supplements is essential to avoid deficiencies that can affect health.
Common supplements post-surgery include:
Doctors will monitor levels regularly through blood tests to adjust dosages as needed.
Staying hydrated is vital for overall health, especially after gastric sleeve surgery. Dehydration is common due to the reduced stomach size limiting fluid intake at one time.
Patients should aim for at least 64 ounces of fluid daily but avoid drinking 30 minutes before or after meals to prevent overfilling the stomach pouch.
Some foods may now cause discomfort or complications such as nausea, bloating, diarrhea, or constipation post-surgery.
Foods often avoided include:
Listen to your body's signals when introducing new foods into your diet post-operation.
Laparoscopic gastric sleeve surgery (LSG) is a significant procedure with potential risks and complications. It's crucial to know these before deciding on surgery.
Every surgical procedure has short-term risks. With LSG, these can include infection, bleeding, and adverse reactions to anesthesia. Immediately after surgery, patients might experience pain or discomfort as they recover. Although rare, there could be issues with the staples used in the stomach, leading to leaks at the staple line.
Doctors monitor patients closely following LSG to manage any immediate complications. Hospitals have protocols to minimize risks such as administering antibiotics to prevent infections and using techniques that reduce bleeding during surgery.
Long-term complications from LSG are less common but can be serious. Some patients may develop nutritional deficiencies due to the reduced size of their stomachs. This makes it harder for them to absorb certain vitamins and minerals.
Another possible long-term issue is gastroesophageal reflux disease (GERD), which can cause heartburn and discomfort. In some cases, weight regain can occur if lifestyle changes are not maintained post-surgery.
Patients should engage in regular follow-ups with their healthcare provider to ensure they're managing their nutrition properly and addressing any long-term issues that arise.
Major complications from LSG include deep vein thrombosis (DVT), pulmonary embolism, or a severe reaction known as stricture where the stomach becomes too narrow. These are rare but require immediate medical attention.
Statistically speaking, major complications occur in a small percentage of cases; however, understanding these risks is essential for informed consent before undergoing LSG.
Healthcare providers will assess individual risk factors like age, overall health status, and obesity-related conditions before recommending this surgery.
Reducing the risks associated with LSG involves several steps both before and after surgery. Preoperative evaluations help identify any existing health concerns that could complicate surgery or recovery.
Postoperatively, adherence to dietary guidelines helps prevent complications related to nutrition deficiency or overeating which could strain the new stomach size. Regular exercise also plays a critical role in maintaining weight loss and overall health post-surgery.
Surgeons with extensive experience in laparoscopic procedures tend to have lower complication rates due to their expertise in handling potential issues during surgery.
After understanding the risks and complications associated with Laparoscopic Gastric Sleeve (LSG) surgery, it's crucial to focus on the lifestyle changes needed for successful weight loss. This section will delve into how patients can adapt their daily habits post-surgery.
Following LSG, your diet will undergo significant changes. Initially, you'll start with a liquid diet before gradually reintroducing solid foods. This progression is vital for proper healing. Over time, eating small, balanced meals becomes the norm. Patients must prioritize high-protein foods while reducing sugary and fatty items to maximize weight loss.
Portion control is also essential since the stomach's capacity is reduced. Here are some dietary guidelines:
Regular physical activity is another key aspect of life after gastric sleeve surgery. Exercise aids in maintaining muscle mass during rapid weight loss and boosts metabolism. Most importantly, it helps sustain long-term weight management.
Start with low-impact activities like walking or swimming as recommended by your healthcare provider. Gradually increase intensity as your body adjusts. Aim for at least 150 minutes of moderate aerobic activity per week.
Tracking your progress post-surgery keeps you motivated and informed about your health status. Regular check-ins with your doctor help ensure you're losing weight safely and can address any concerns promptly.
Patients typically experience rapid weight loss initially, which slows down over time. On average, individuals can expect to lose 60% of their excess weight within two years post-surgery.
Significant weight loss from LSG may lead to improvement or resolution of obesity-related conditions such as sleep apnea. Patients often report better sleep quality and reduced daytime fatigue once they've shed a substantial amount of weight.
It's important to continue working closely with medical professionals to monitor these conditions even after experiencing improvements.
Laparoscopic gastric sleeve surgery (LSG) has changed many lives. Individuals who once struggled with obesity now enjoy improved health and vitality. These real-life transformations are not just about weight loss. They represent a new chapter in people's lives, filled with activities they could not participate in before.
One example is Sarah, a 42-year-old woman who underwent LSG. She lost over 100 pounds within a year post-surgery. Before LSG, Sarah dealt with high blood pressure and type 2 diabetes. Now, her blood sugar levels are normal, and she no longer needs medication for hypertension.
The health benefits of SG extend beyond weight loss. Patients often experience significant improvements in obesity-related conditions such as diabetes, sleep apnea, and joint pain.
Studies show that SG can lead to remission of type 2 diabetes in many cases. This is due to the surgery's impact on gut hormones that influence insulin secretion and blood sugar control.
Those who suffer from sleep apnea may find relief after SG because weight loss can reduce airway obstruction during sleep. Joint pain also tends to decrease as there is less stress on the body's support structures.
Weight loss surgery like SG can have profound effects on psychological well-being too. The improvement in appearance often boosts self-esteem and confidence.
A survey conducted among post-SG patients revealed that many reported better mental health outcomes. They felt more socially active and less anxious about public perception of their bodies.
However, it is essential to note that psychological support should accompany physical changes for sustainable results.
Long-term success rates of SG are promising when paired with lifestyle changes discussed earlier. Consistent follow-up care ensures that patients maintain their weight loss achievements.
Statistics indicate that most patients keep off at least 50% of their excess weight five years after surgery. This success rate underscores the importance of ongoing commitment to dietary adjustments and exercise routines initiated post-surgery.
Laparoscopic gastric sleeve surgery stands as a transformative procedure for those battling with obesity, offering a path to sustainable weight loss and improved health outcomes. This article has journeyed through the eligibility criteria, detailed the surgical process, highlighted the benefits, and underscored the necessary preparations and postoperative care. It has also illuminated the dietary modifications required, addressed potential risks, and showcased inspiring success stories. The collective insights affirm that while sleeve gastrectomy can be life-altering, it demands a commitment to long-term lifestyle changes.
For individuals contemplating this weight loss surgery, it is imperative to consult with healthcare professionals to understand its suitability for their unique circumstances. As you weigh your options, remember that the decision to undergo laparoscopic sleeve gastrectomy should be made with careful consideration of both its possibilities and obligations. If you're ready to take the next step towards a healthier future, reach out to a qualified bariatric surgeon today.
Candidates typically have a BMI over 40 or a BMI over 35 with obesity-related health conditions. Physician assessment is required.
The procedure involves removing approximately 80% of the stomach, creating a tube-like structure, using minimally invasive techniques.
Recovery time varies but generally, patients return to normal activities within 2-4 weeks post-surgery.
Benefits include significant weight loss, improved obesity-related conditions, and minimal scarring due to small incisions.
Post-surgery diets start with liquids, progressing to pureed foods, then soft foods, and finally regular food in smaller portions.
Yes, potential risks include bleeding, infection, and nutritional deficiencies. Consultation with a healthcare provider is essential.
Yes. Adopting a healthy diet and regular exercise routine can improve weight loss outcomes and overall health after surgery.